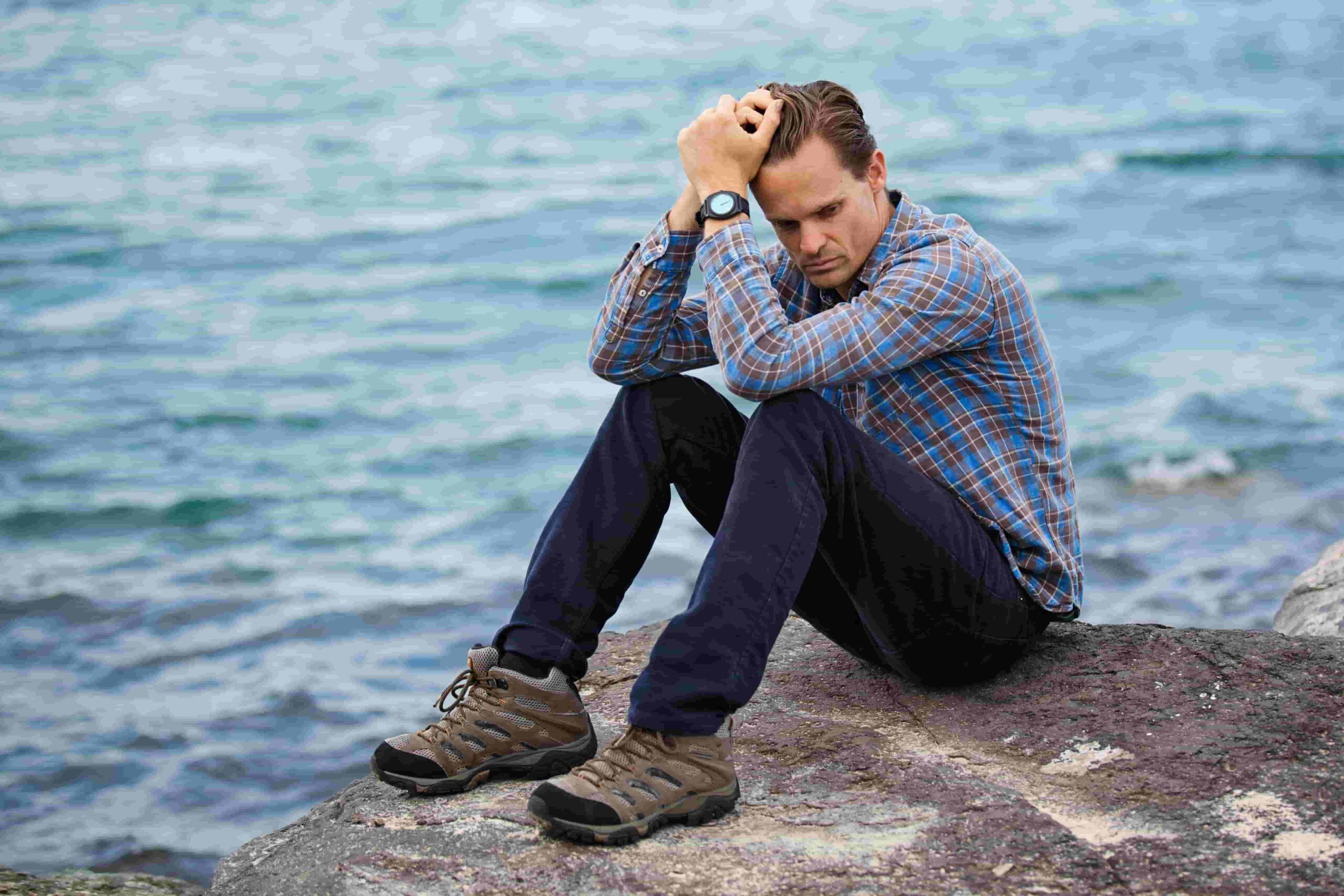
CPTSD and depression, what is the connection between them?
Complex post-traumatic stress disorder (C-PTSD) is a diagnosable condition typically triggered by a series of ongoing traumatic events — often during childhood. Depression is much more than feeling the blues. It’s also a diagnosable disorder and it can be associated with C-PTSD. Before we continue, let’s be clear that experiencing chronic trauma is not a guarantee of C-PTSD. Also, being diagnosed with either depression or C-PTSD does not make it inevitable that you will struggle with the other.
Simply put, there’s a connection between the disorders that must be taken into account when assessing symptoms. In particular, someone with C-PTSD is more likely to be diagnosed with depression than someone with post-traumatic stress disorder (PTSD).
The Connection Between CPTSD and Depression
 People with PTSD are impacted by enduring or witnessing a horrific event. With CPTSD, however, the root cause lies in multiple such events. From abandonment to domestic violence to all types of abuse and beyond — complex trauma survivors undergo experiences from which they cannot escape — often at the hands of people they know.
People with PTSD are impacted by enduring or witnessing a horrific event. With CPTSD, however, the root cause lies in multiple such events. From abandonment to domestic violence to all types of abuse and beyond — complex trauma survivors undergo experiences from which they cannot escape — often at the hands of people they know.
This type of scenario can change how one’s brain processes thoughts, memories, and emotions. At the same time, the survivor can develop a very negative self-image. When seeking treatment, signs like this are logically assigned to complex trauma. That said, the presence of shame and guilt could also be pointing to a major depressive disorder (MDD).
Making such a distinction is crucial. After all, a major symptom of MDD is suicidal ideation. Thus, if depression is not identified, important steps to address the possibility of self-harm may not be taken.
Recognizing a CPTSD and Depression Co-Morbidity
It starts with ruling out medical causes for symptoms while also looking for PTSD. The overlap of PTSD and C-PTSD symptoms is large so only an extensive assessment can differentiate. Taking a full history can help reveal the specific events that brought the person to their current state.
C-PTSD alone frequently manifests in signs that do not indicate depression. These include intrusive memories, hyper-arousal, and nightmares. Meanwhile, all of depression’s symptoms can possibly be observed in a complex trauma. However, it is the tendency toward self-harm and suicide attempts that is more escalated in people with MDD.
Therefore, besides a full history being taken, a practitioner may rely on observation, questionnaires, and conversations with people who know the person in question. In addition, it’s important to consider biological and risk factors.
Biology
Trauma can damage parts of your brain. This reality leads to changes in how you manage emotions and deal with triggers. Hence, a comprehensive exam can be indispensable when either C-PTSD or depression (or both) are suspected to be present. How a person responds to stress, makes decisions, and more can be quite revealing in this process.
Risk Factors
As mentioned, exposure to traumatic events (especially during childhood) is the primary risk factor for C-PTSD. Other elements to explore include:
- Socioeconomic status
- Education level
- The presence of high anxiety or an anxiety disorder
- A family history of mental illness
- Lack of social support
As you can surely discern by now, the work of diagnosis is deliberate and all-encompassing. This is necessary because living with both C-PTSD and depression, increases your odds of struggling with:
- Related physical issues
- Relationship problems
- Financial struggles
- Substance abuse
- Shame, guilt, hopelessness, and high levels of stress
CPTSD and Depression Can Be Treated and Managed
To help you disentangle yourself from CPTSD and depression, you’ll need a professional who is experienced with trauma and co-morbidities. With such help, you can find the right treatment plan (self-care, therapy, medication, etc.) to manage symptoms while directly addressing the two disorders. Right now, things may feel confusing and bleak. With the proper guidance, you can thrive again. Let’s talk about this soon. Reach out to learn more about depression or trauma treatment.